नमस्कार,
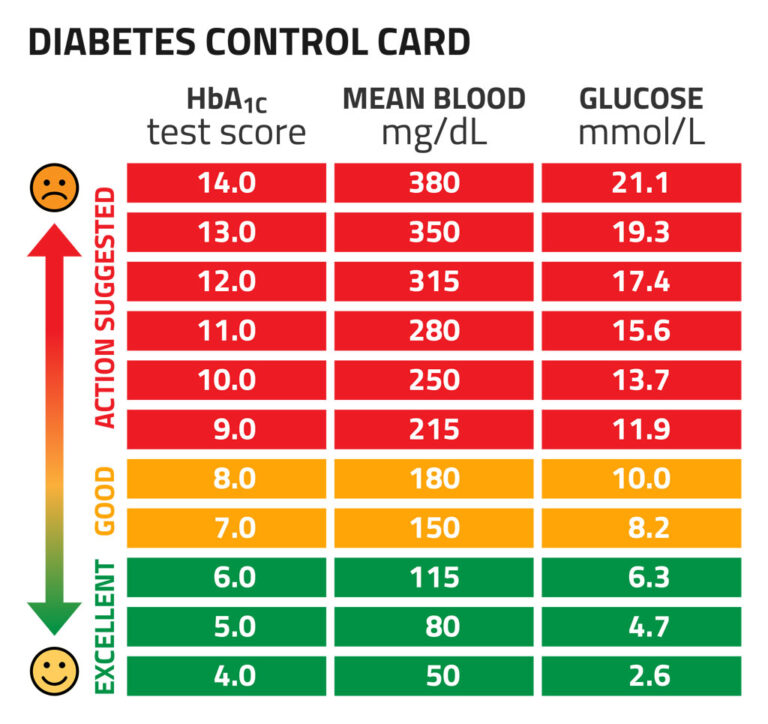
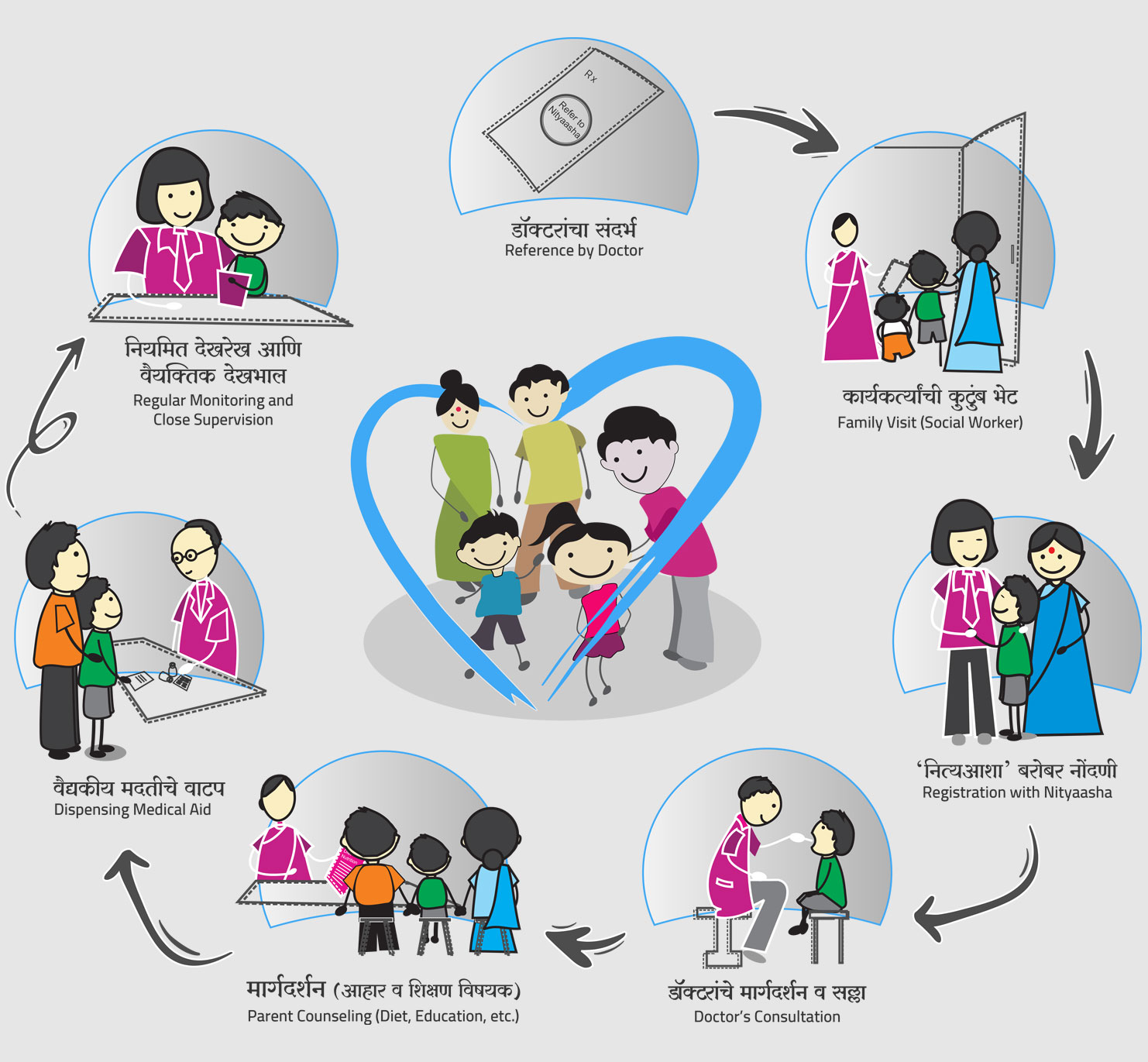
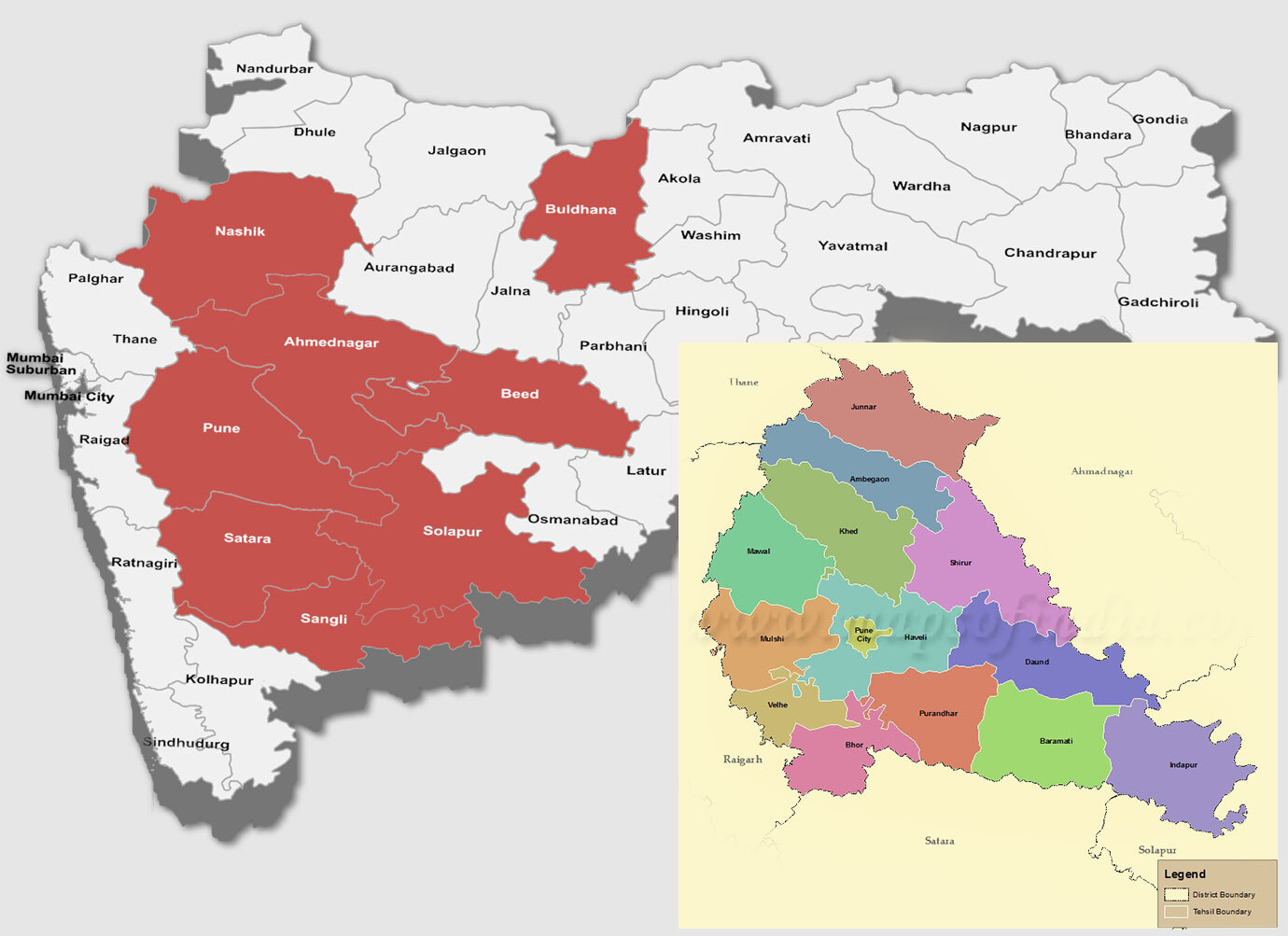
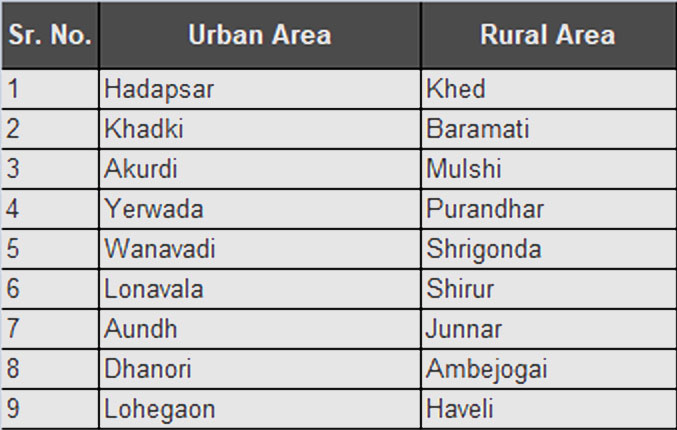
मी राजश्री शंकर सांगळे. मी काही काळ नित्याशा फाउंडेशन ची सदस्य होते. मला इथे खूप छान अनुभव मिळाला. डायबेटिस हा आजार आयुष्यभर आपल्या सोबत असणार आहे तेंव्हा याला आपला सखा सोबती समजून कसे सांभाळायचे आणि कशी काळजी घ्यायची हे मी इथे शिकले. कौटुंबिक वातावरण आणि डायबेटिस यांची नाळ कशी जुळते हे देखील समजले. नित्याशा फाउंडेशन आर्थिक दृष्ट्या दुर्बल कुटुंबातील डायबेटिस झालेल्या व्यक्तीला वैद्यकीय मदत तसेच तज्ञ डॉक्टरांतर्फे मार्गदर्शनाचे मोठे कार्य करते. माझ्या कुटुंबाला आणि मला केलेल्या मदतीबद्दल तसेच इतर जीवनावश्यक गोष्टी मिळवण्यासाठी मार्गदर्शन केल्याबद्दल मी त्यांची खूप खूप आभारी आहे.
– राजश्री शंकर सांगळे